Labor Induction
When a pregnant woman is unable to continue pushing or when a caesarean section (C-section) is not feasible, labor may be induced. Labor induction is a procedure to stimulate uterine contractions before labor begins naturally. The causes for labor induction include:
Approaching 2 weeks beyond due date
Labor hasn’t started naturally
Water has broken, but a woman is not having contractions
Infection in the uterus
Baby has stopped growing at expected pace
Lack of amniotic fluid surrounding baby (oligohydramnios)
Leads to lung immaturity
Placenta has begun to deteriorate
Placenta peels away from inner wall of uterus before delivery
Partial or completely
Associated medical condition putting the baby at risk
Diabetes
High blood pressure
Hypo/hyperthyroidism.
Risks associated with labor induction are:
Need for C-section
Premature birth
Low heart rate (bradycardia)
Diminish your baby’s oxygen supply
Infection for mother and baby
Umbilical cord complications
Uterine rupture
Bleeding after delivery.
Labor induction is not for:
Women with prior C-section
Placenta blocking the cervix – placenta previa
Baby is lying crosswise in uterus – transverse fetal life
Active genital herpes infection (HSV 2)
Birth canal too small to allow for normal birth.
The process may only be performed in a hospital with appropriate monitoring. Women who reside in Denver should visit the Denver Holistic Center for more information. Here are some things the physician will do beforehand:
Strip or sweep the amniotic membranes
Ripen the cervix – using synthetic prostaglandins
Manually break a pregnant woman’s water – amniotomy or rupturing the membranes
Intravenous medication – oxytocin to induce labors or prevent hemorrhaging.
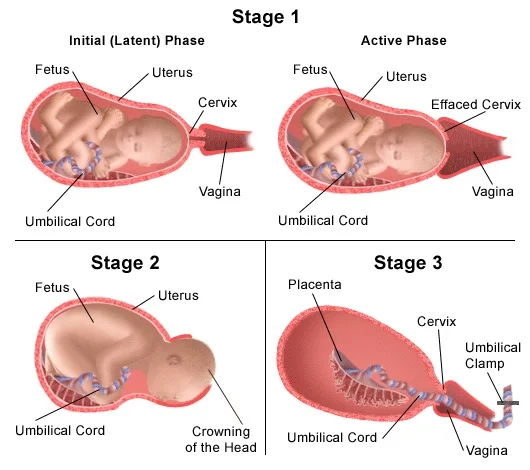
Figure 1 – This is how labor induction is done.
Figure 2 – Different stages of labor.3 Stage I (up to full dilation: Latent Phase [contractions → 4 cm] and Active Phase [4-10 cm]), Stage II (full dilation → Delivery), Stage III (Delivery of the placenta due to PG-F, blood gush → cord lengthens → fundus firms).
Conclusively, this is a risky procedure and each and every pregnant woman should be made fully aware of the risks and impediments.